Research behind the Sapiens Diagnostics
In high-stakes knowledge jobs, peak performance often comes at a cost. The cost is not always visible. Sapiens makes it measurable. We quantify how your biology adapts to stress, where regulation starts to drift, and which routines restore resilience. We base this on top-tier allostatic load science, medical-grade biomarkers, and validated self-assessments.
Research-backed performance support
For most performers, intense cognitive load, constant context switching, travel, sleep disruption, and psychosocial pressure can push the body into a costly “always on” adaptation mode. People often notice it only when it’s already expensive: loss of energy, shallow sleep, irritability, cognitive fatigue, gut issues, recurrent infections, stubborn weight changes, anxiety, or a creeping sense that recovery isn’t working anymore.
Traditional healthcare is excellent at acute problems. Yet, it’s not designed to bring ambitious people from "good" to “great”: Increase energy, sharpen focus, stabilize mood, strengthen recovery. The job of traditional healthcare is efficient disease detection and organ-specific treatment. Chronic stress and human performance on the other hand, by definition, is upstream, multi-system, and slow-moving. It’s real biology, but it doesn’t fit neatly into one specialty.
Thus traditional healthcare focuses on the downstream effects of chronic stress once it has turned into a disease, yet not on chronic stress itself or it's early impacts on the body. Sapiens complements this by supporting high performers from good to great. We also support them through difficult periods of stress, fatigue and overwhelm.
We focus on three steps:
First, we quantify the price your body pays for stress (or the benefit of a resilient system) across multiple systems.
Second, we translate your personal pattern into the next best actions, tailored to your calendar and goals.
Third, we increase the probability that new routines survive busy periods through habit-change support and re-measurement.
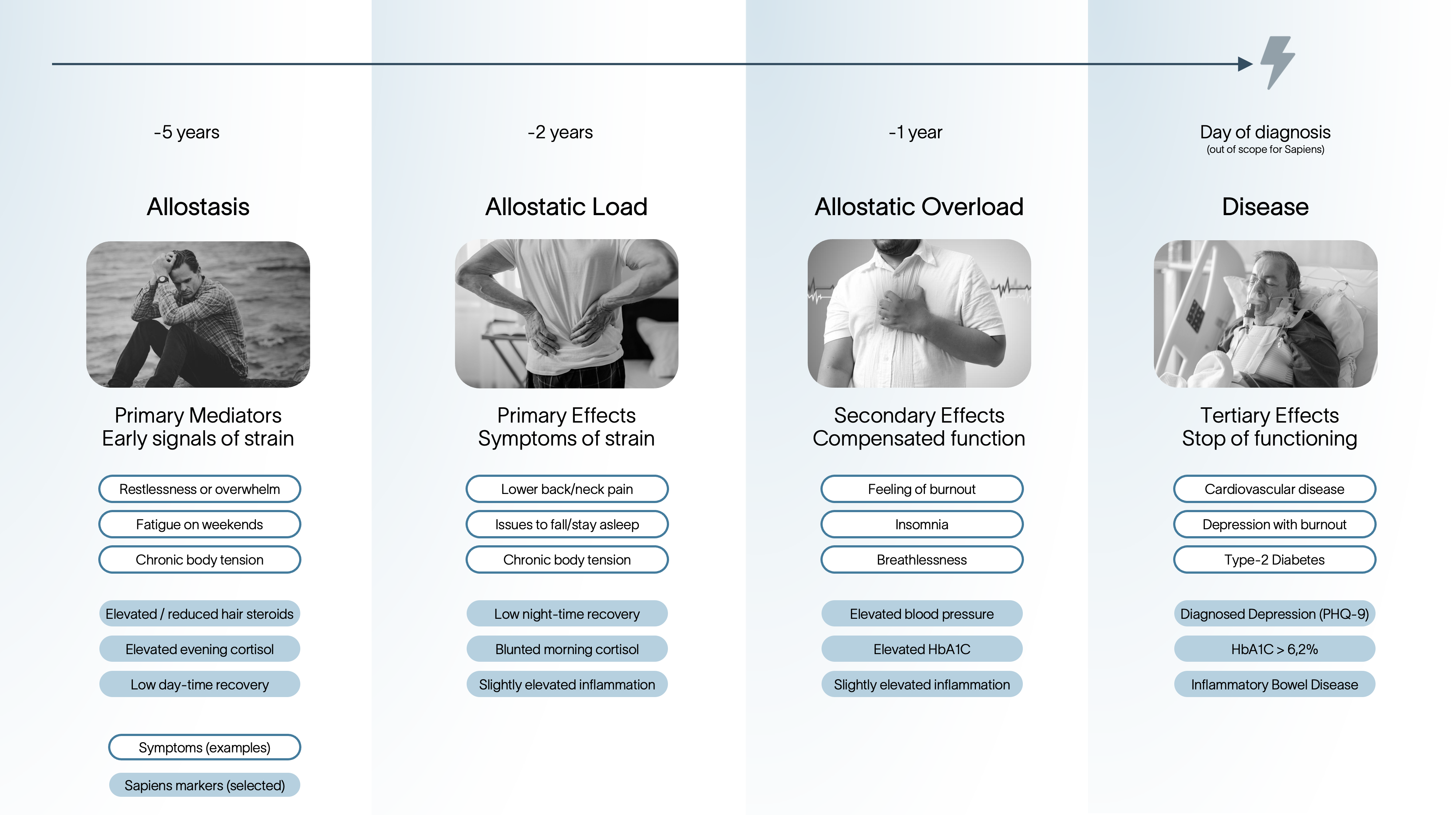
The Allostatic Load Model
The Sapiens diagnostics is built around the Allostatic Load Model. The allostatic load model was initiated by Bruce McEwen (1993) to measure the “price” your body pays for stress. Today 350+ peer reviewed publications have refined, tested and validated the model. The main insight of the allostatic load model: Stress mediators like Cortisol can be helpful in the short term, but damaging to health and performance when activation is repeated or persistent.
Allostasis means “stability through change.” The brain predicts demands and adjusts physiology to meet them. It uses stress-mediating systems such as the HPA axis (e.g., cortisol) and the autonomic nervous system (sympathetic/parasympathetic balance) to initiate the adaptation to stress. It also shifts the immune system, gut functioning and metabolic signaling. These adaptations are supposed to support performance and health on the short-term (McEwen & Seeman, 1999). When high demand persists and recovery is insufficient, short responses of the bodies stress systems turn into persistent states. The measurable result is multi-system dysregulation (e.g., less ability to focus, more fatigue, suboptimal gut health and higher emotional reactivity). That cumulative burden is called allostatic load.
Disease and performance declines don't appear suddenly, but are following 4 steps:
Step 1 - Allostasis: Short-term activation to meet a demand (e.g., cortisol elevation), followed by recovery.
Step 2 - Allostatic load: Repeated or prolonged activation of the bodies stress systems create cumulative, measurable dysregulation across body systems.
Step 3 - Allostatic overload: Dysregulation becomes clinically meaningful dysfunction and long-term disease risk rises.
Step 4 - Diseases: Once selected body systems no longer have the resources to deal with the overload, diseases may arise
The Sapiens Body Reserve Score
Sapiens leverages the Allostatic Load Index that has been operationalized through 60 peer-reviewed publications as a composite, multi-system risk score. The Allostatic Load Index is widely used in population and aging research because it predicts hard downstream outcomes, not just “stress feelings.” In the original MacArthur work and subsequent cohorts, higher allostatic load scores predicted all-cause mortality, declines in physical functioning, and declines in cognitive functioning, and showed associations with incident cardiovascular events, even after adjusting for sociodemographics and baseline health (Seemann et al., 2001). A large systematic review found that high allostatic load is associated with higher risk of all-cause mortality and cardiovascular mortality, supporting prognostic validity at scale (Parker et al., 2022). Also, the Allostatic Load Index has been established in occupational settings (Mauss et al., 2014).
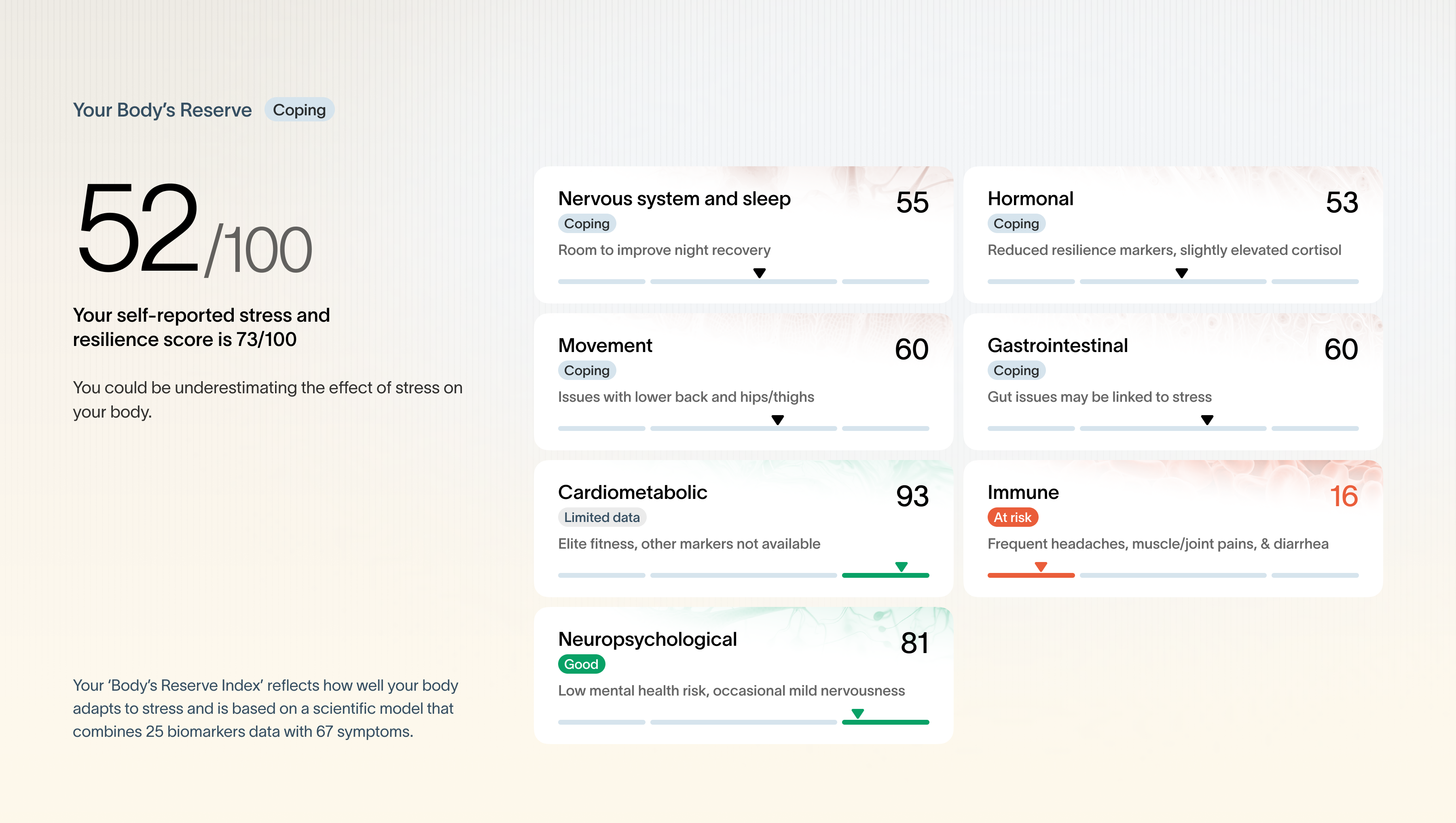
Sapiens integrates the approaches from the Allostatic Load Index literature as also reviewed by Carbone et al., in 2022, and further refines them by collarborating with the researchers behind these methods like Professor Robert Paul Juster. By measuring allostatic load, Sapiens intervenes upstream of disease and performance decreases. We first measure the state of the two core stress-mediating systems - nervous system regulation and hormonal regulation - to quantify strain and regulatory capacity. Then we assess downstream effects in stress-sensitive body systems (e.g., immune, cardiometabolic, gut, neuropsychological). The more downstream systems show strain while stress mediators are dysregulated, the higher the inferred “price,” and the lower the Body Reserve score.
Sapiens works with top-tier scientists
To operationalize the allostatic load model, we are collaborating with top-tier scientists and former medical doctors that bring practical experience.
For example, Prof. Clemens Kirschbaum has published over 500 peer-reviewed articles in the field of stress research and has a Google Scholar h-index of 150 and is a leading researcher on stress hormones. His work helped establish how cortisol is measured and interpreted in research and real life. We collaborate with Dresden LabService for hormone analytics from hair and saliva. DresdenLab Service is a spin-off from Technical University Dresden and a globally leading stress hormone research laboratory with 20 years of experience.
Prof. Robert-Paul Juster is a leading researcher in chronic stress and allostatic load biology, including how multi-system biomarkers relate to health trajectories.
Our internal team includes Julian Scherer (ETH Zürich, Biotechnology), Prejwal Prabhakaran (Freiburg University, Neuroscience), Dr. Andrea Allgäuer (PhD Biotechnology and Immunology), and practitioners such as Dr. Dominique Sauter-Peschke (Medical Doctor) and Ellis Broeks (Medical Doctor).
Sapiens measures biomarkers of stress and health-impact of stress
Stress and health cannot be captured with a single marker because stress is a multi-system process. An influential syntheses by Robert-Paul Juster (advisor to Sapiens) and colleagues, consolidated why allostatic load is best treated as a multi-system pattern: chronic stress exposure produces coordinated shifts across neuroendocrine, autonomic, immune, metabolic, and cardiovascular systems, and combining markers better captures cumulative strain than any single readout (Juster et al., 2009).
This shows the limitations of wearbles, as single biomarkers miss the biology of chronic stress. Even though they are called “stress monitors,” wearables such as Oura, Whoop, or Garmin only measure a narrow slice of nervous system function. HRV reflects a limited window into autonomic (nervous system) regulation and short-term physiological load, but it does not directly capture hormonal dynamics, which are often more sensitive to psychosocial stress.
Sapiens therefore measures both major stress-mediating systems - the autonomic nervous system and the HPA axis (stress hormones) - across multiple time windows. We quantify longer-term strain using 3-month hair steroid analysis, and shorter-term regulation using multi-day salivary cortisol profiles. We then triangulate these upstream mediator signals with markers and symptoms from stress-sensitive downstream systems - such as the immune, gastrointestinal, neuropsychological, cardiometabolic, and musculoskeletal systems—to estimate the total “price” the body is paying for stress.
Overall, we combine up to these biomarkers from multiple biosamples:
Hair steroids: cortisol, cortisone, DHEA, testosterone, progesterone, plus selected ratio biomarkers
Hair endocannabinoids (research-frontier markers, interpreted cautiously): AEA, 2-AG, PEA
Saliva cortisol rhythm (2–3 days): Waking Cortisol, +30 min Cortisol and pre-bed Cortisol to capture mechanisms of cortisol regulation
Multi-day ECG recovery analytics: HR and HRV-derived stress–recovery patterns and sleep recovery dynamics
Optional tests (case-dependent): blood markers such as inflammation and micro-nutrients, glucose monitoring, microbiome testing (research-frontier marker), blood pressure
We triangulate biomarkers with scientifically validated self-assessments
Biomarkers alone does not explain everything and often miss context. Two people can have similar physiology for different reasons. We add validated instruments to capture domains biology alone cannot resolve: perceived stress, resilience, fatigue, sleep quality, burnout risk, mood and anxiety screening, work environment, and symptom burden across body systems (e.g., GI, immune, musculoskeletal). We also capture confounders that change interpretation (sleep timing, travel, illness, alcohol, medication exposure). We use only scientifically validated questionaires such as Brief Resilience Scale, Maslach Burnout Inventory, GAD-7 for anxiety etc.
As we are measuring allostatic load and don't measure direct disease markers we are offering this as a wellness service, not as a medical service. Yet, we are deplyoing medical-grade standards throughout our offering.






